-
PROVIDERS
New MRD Medicare Coverage for Select Indications*
*When coverage criteria are met. Additional criteria and exceptions for coverage may apply.
-
LIFE SCIENCES
ENROLL NOW
Tempus’ patient-derived organoid screens
Evaluate the efficacy of your preclinical compounds using fixed organoid panels designed for diverse therapeutic applications -
PATIENTS
It's About Time
View the Tempus vision.
- RESOURCES
-
ABOUT US
View Job Postings
We’re looking for people who can change the world.
- INVESTORS
05/20/2024
Structured EHR Data Underestimates Prevalence and Misses Large Proportions of Patients With Pulmonary Hypertension
ATS 2024
PRESENTATION
Authors
R. Chen, J. Pfeifer, D. Leibowitz, D.M. Vidmar, W. Thompson, J. Leader, K. Morland, A. Nelsen, B. Fornwalt
Rationale – Pulmonary hypertension (PH) is a progressive, debilitating disease with increasing treatment options. However, identifying PH patients in real-world datasets is challenging, thereby limiting efforts to optimize medical therapy and improve clinical research, including generating accurate estimates of population-wide prevalence. We sought to determine whether patients with PH could be reliably identified using structured electronic health record (EHR) data and estimate population-wide prevalence.
Methods – Using a longitudinal de-identified EHR dataset of over 2 million patients, we first developed a filtering method to remove patients without any evidence of disease or possible disease across multiple data modalities. This enables random sampling for a reliable estimate of sensitivity within a feasible number of chart reviews. From the remaining cohort(filtered population), we randomly sampled 300 patients for a blinded, two-physician review to identify those with clinically diagnosed defined as a clear diagnosis or mentioned in the unstructured note text by a clinician. We then characterized the availability of structured data elements, including any occurrence of a PH diagnosis code on the problem list or in any encounter, any order or medication reconciliation of PH-specific vasodilator therapies, or any right heart catheterization (RHC) with mean pulmonary artery pressure >20mmHg. Additionally, we calculated an estimate for population-wide prevalence by extrapolating the proportion of true positives within the random sample of the filtered population to the entire EHR population; this conservatively assumes all patients outside the filtered population are disease-free, ensuring we do not overestimate true prevalence.
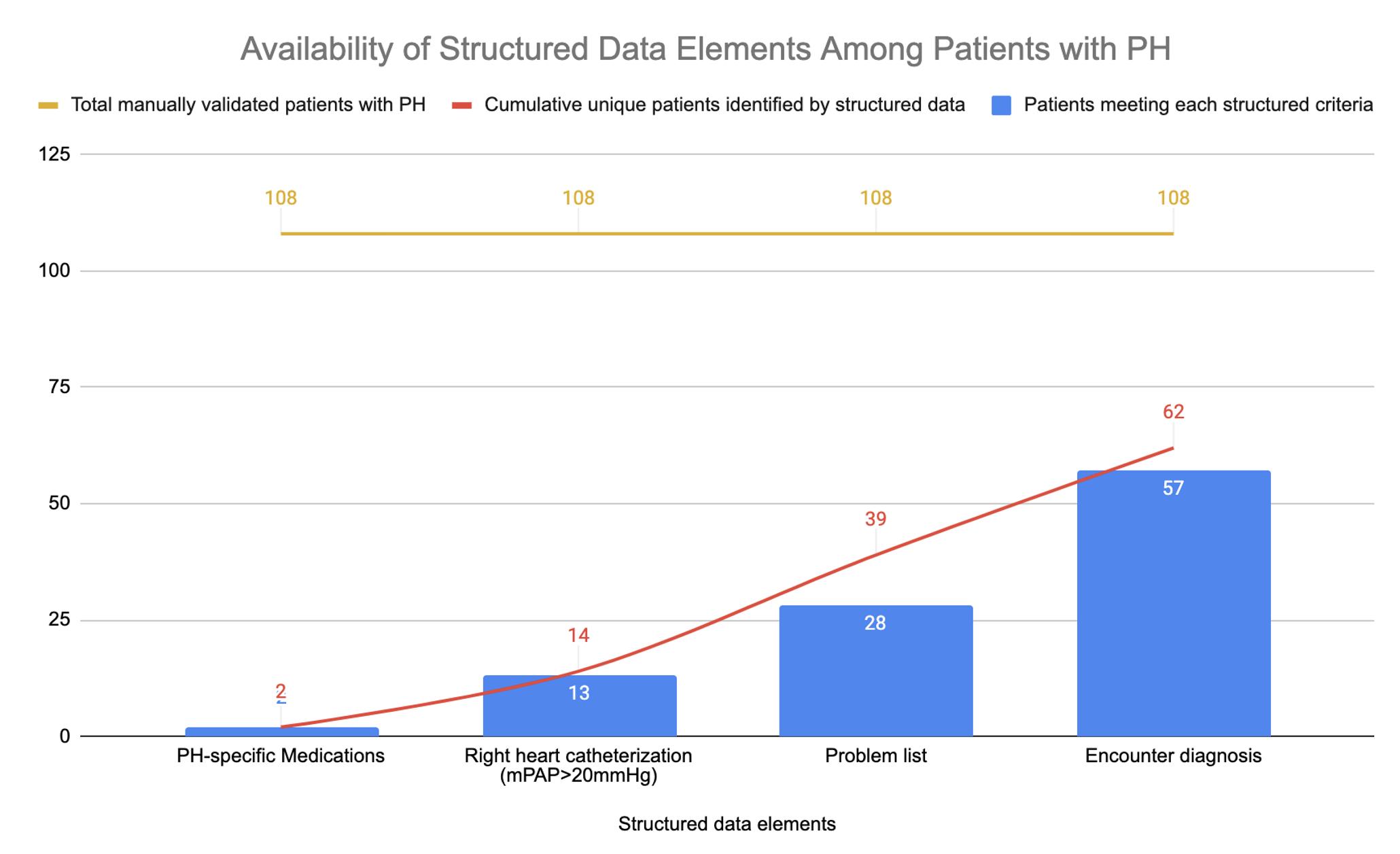
Results – Within the random sample of the filtered population, we identified 108 patients with clinically diagnosed PH, of which only 57%(62/108) had any structured data elements suggestive of PH (Figure). Specifically, only 26% of patients had a PH code on their problem list, 53% had a PH encounter diagnosis code, 2% were on a PH medication, and 12% had a RHC meeting diagnostic criteria. Overall, 43% of patients did not have any structured EHR data suggestive of PH yet were noted to have clinically diagnosed PH in unstructured note text. The population-wide prevalence of PH was estimated to be 2.4%, which is higher than the∼1% estimate in existing literature.
Conclusions – Structured data elements in EHR datasets fail to identify a large proportion of patients with clinically diagnosed PH. Leveraging unstructured data from clinical notes, such as in natural language processing-based phenotyping approaches, may be necessary for more complete identification of patients with PH in EHR data.