-
PROVIDERS
New MRD Medicare Coverage for Select Indications*
*When coverage criteria are met. Additional criteria and exceptions for coverage may apply.
-
LIFE SCIENCES
ENROLL NOW
Tempus’ patient-derived organoid screens
Evaluate the efficacy of your preclinical compounds using fixed organoid panels designed for diverse therapeutic applications -
PATIENTS
It's About Time
View the Tempus vision.
- RESOURCES
-
ABOUT US
View Job Postings
We’re looking for people who can change the world.
- INVESTORS
11/05/2024
Impact of Timing of Real-World CT Imaging on Cost-Effectiveness of a Molecular Biomarker for Treatment Response Monitoring of Immunotherapy
SITC 2024
PRESENTATION
Authors
Zach Rivers, Charu Aggarwal, Marc Matrana, Akash Mitra, Halla Nimeiri, Rotem Ben-Shachar, Sheetal Kircher
Background
Studies have demonstrated that dynamic molecular biomarkers for treatment response monitoring (TRM) of immune checkpoint inhibitors (ICI) can predict clinical outcomes. However, there is little data on when a molecular biomarker is best integrated into clinical practice based on timing of Computed Tomography (CT) imaging. Here, we characterize real-world (RW) imaging patterns in a cohort of advanced pan-cancer patients treated with ICI. We model the impact of these patterns on the clinical utility and cost-effectiveness of a molecular biomarker for TRM compared to imaging.
Methods
We analyzed CT scan frequency in linked Tempus AI clinicogenomic and Komodo Health claims databases. Patients were evaluable if they were diagnosed with Stage 3B, 3C or 4, received first line ICI +/- chemotherapy for ≥60 days, and received ≥2 CT scans. Previously, we published a microsimulation of advanced cancer patients treated with IO that compared the use of xM, a molecular biomarker for TRM, in conjunction with rw-maging (intervention) to imaging alone (control).1 We assume that all treatment decisions occur after CT imaging; in the intervention group, molecular non-responders switch to chemotherapy and molecular responders remain on ICI; in the control group, treatment switching decision is determined by the imaging result only. We updated the model to incorporate rw-imaging frequency within 24 weeks of ICI therapy. Median CT scan interval difference by treatment and cancer type was tested using the Kruskal-Wallis test. We calculated total treatment and molecular testing costs from Medicare’s perspective.
Results
Across five solid cancers, 4,147 patients were evaluable for the RW-imaging analysis. Median scan intervals were significantly different across treatment and cancer subtype (tables 1, 2), with first scans ranging from a median of 48 days (SCLC treated with IO+chemo) to 80 days (melanoma patients treated with IO). When we incorporated this data into the simulation model, intervention patients receiving earlier scans (range: 6–11 weeks) had greater per-patient total cost savings ($4,700 to $7,100) and longer weeks of inappropriate therapy avoided (4.3–5.8) over a 24 week period compared to the control patients (figure 1).
Conclusions
Utilization of RW-imaging varies across cancer types and therapy. Despite the heterogeneity in rw-imaging, xM for TRM in conjunction with imaging remained cost-saving compared to CT imaging alone across all cancer subtypes. The greatest cost savings and weeks of inappropriate therapy avoided was seen in advanced SCLC treated with ICI-chemotherapy, where rw-imaging occurs at more frequent intervals than others.
Reference
- Rivers, et al. Cost-effectiveness of a circulating tumor fraction molecular biomarker for treatment response monitoring. Journal of Clinical Oncology. 2024;42:16


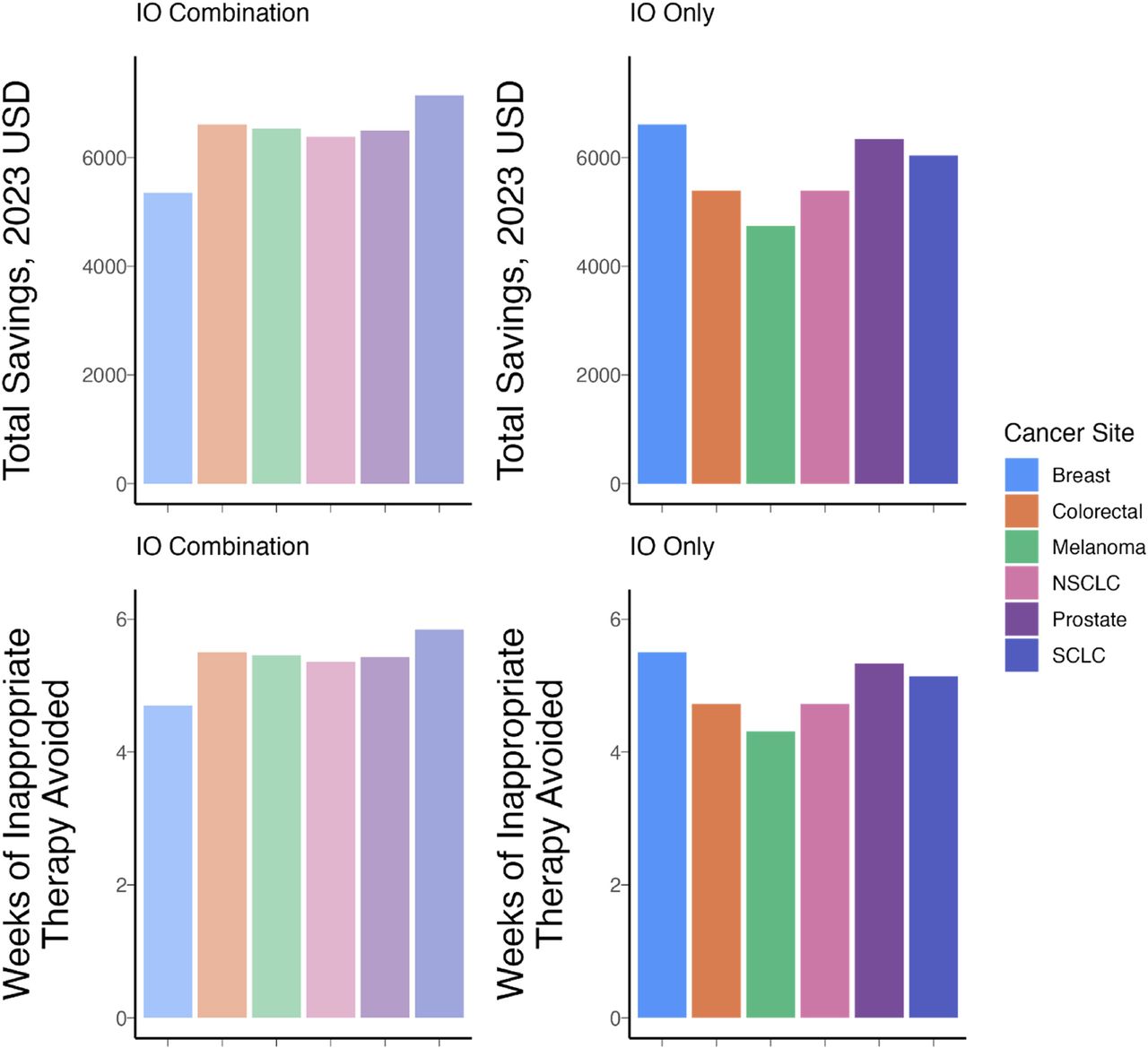
Figure 1 – Total costs and weeks of inappropriate therapy avoided by cancer type