-
PROVIDERS
New MRD Medicare Coverage for Select Indications*
*When coverage criteria are met. Additional criteria and exceptions for coverage may apply.
-
LIFE SCIENCES
ENROLL NOW
Tempus’ patient-derived organoid screens
Evaluate the efficacy of your preclinical compounds using fixed organoid panels designed for diverse therapeutic applications -
PATIENTS
It's About Time
View the Tempus vision.
- RESOURCES
-
ABOUT US
View Job Postings
We’re looking for people who can change the world.
- INVESTORS
10/11/2023
Five key learnings regarding clinical and research applications of liquid biopsy
Scientific and medical leaders from Tempus discuss the evolution of liquid biopsy in clinical practice and development.
Authors
Nike Beaubier, MD
SVP, Life Science Pathology, Tempus

Ezra Cohen, MD
Chief Medical Officer of Oncology, Tempus

SVP, Life Science Pathology, Tempus

Ezra Cohen, MD
Chief Medical Officer of Oncology, Tempus

Tempus recently announced the release of its expanded liquid biopsy panel, xF+, one of the largest clinically available comprehensive genomic profiling tools on the market. As a robust liquid biopsy panel, xF+ can detect gene alterations and resistance mechanisms in cell-free DNA, complementing traditional tissue biopsy testing methods. In a recent webinar, three scientific and clinical leaders from Tempus discussed the evolution of liquid biopsy in clinical practice and development.
Below, we share five key learnings from the discussion between Dr. Nike Beaubier, SVP, Life Science Pathology, Dr. Ezra Cohen, Chief Medical Officer of Oncology, and Mike Yasiejko, General Manager and EVP, in addition to their insights on the future of liquid biopsy utility across early- and late-stage clinical development.
For their full discussion, watch the webinar recording here.
#1 Expanded liquid biopsy panels streamline therapy response monitoring
With technical improvements and a lower cost of sequencing, liquid biopsy panels have improved the pace of genomic profiling in research and clinical development. Dr. Beaubier highlights large panels with the capacity to sequence as many as 523 genes as relatively new in the liquid biopsy space. Panels of this size can provide much more genomic space to calculate tumor mutational burden(TMB), surpassing the roughly 300-gene threshold necessary for accuracy in TMB calculation.
When collecting repeat tissue biopsies during clinical trials is not feasible — either due to tumor exhaustion, body site accessibility, or patient health risks — liquid biopsy sampling simplifies the collection of genetic material and samples from all metastatic sites. “Liquid biopsy mitigates the need to collect tumor samples from high-risk neutropenic and immunosuppressed patients,” said Dr. Beaubier, also citing lung cancer patients with COPD as being at risk for developing pneumothoraces in response to tissue procurement.
“Liquid biopsy testing provides a good view of emerging resistance mutations in response to therapy based on the overall tumor burden measured by median variant allele fraction (VAF) or circulating tumor fraction estimate (ctFE),” explained Dr. Beaubier. “Because of these characteristics, you can sometimes find mutations in liquid biopsy that aren’t detected via tissue testing and vice versa.”
Using liquid biopsy to conduct diagnostic tissue testing alongside longitudinal monitoring provides a comprehensive view of the mutational landscape and response to therapy over time.
#2 ctFE and MRD are both valuable metrics for tumor response monitoring
Circulating tumor fraction estimate (ctFE) is the fraction of cell free DNA (cfDNA) that originates from the tumor, i.e. the fraction of circulating tumor DNA (ctDNA) of all cfDNA. Monitoring ctFE levels enables longitudinal therapy response monitoring in late-stage and advanced cancer patients, where it’s critical to assess stage-dependent metastasis. This is a robust measurement because it is stable with respect to CHIP and germline mutations.
Similarly, minimal residual disease (MRD) is used to monitor tumor response, particularly following curative intent procedures — such as surgical resection or chemotherapy radiation — when the amount of disease in the body is expected to be extremely low, if not zero. As such, MRD is particularly useful in detection of early-stage cancer due to its increased sensitivity.
#3 Liquid biopsy testing complements traditional tissue sampling
Whether in research or clinical practice, liquid biopsy assays complement tumor biopsies and provide greater precision and individualization of therapy.
“Often, we find different sets of mutations from conducting these two types of assays,” explained Dr. Cohen. “And if you think about it, the tumor biopsy is sampling a small piece of a heterogeneous tumor, whereas, with the liquid biopsy samples, the genetic material is shed from the entire tumor mass into the blood.”
Obtaining more information about each patient’s unique tumor profile speeds up the organization and delivery of the appropriate therapeutic interventions.
“If a mutation is found through liquid biopsy and not through tumor sampling, we often believe the finding from the liquid biopsy and can act upon it,” Dr. Cohen added. Dr. Cohen pointed to the faster development timelines of liquid biopsy versus tissue biopsy as critical for expeditious therapy intervention and management.
Compliance with liquid biopsy sampling is much easier for clinical sites during trials, allowing them to monitor drug response and evaluate resistance mutations and tumor burden at an ideal cadence — making trials faster and more nimble.
#4 ctDNA-based therapy response supports patient stratification within clinical trials
Using liquid biopsy to monitor ctDNA levels provides an earlier indication of response to treatment compared to traditional methods of radiology scans or evaluation of biomarker levels.
“Liquid biopsy testing supports monitoring of patients likely to develop resistance earlier, as well as those receiving targeted therapies where these resistance alterations often develop months ahead of clinical progressive diseases typically observed on radiographs,” explained Dr. Cohen. “ctDNA-based monitoring also enables clinical trials to consider early interventions that can extend these patients’ disease-free survival interval.”
Dr. Cohen added that tracking therapy response via ctDNA can help clinicians stratify patients enrolled in clinical trials, especially when evaluating absolute levels of ctDNA for specific alterations and their change over time. Such stratification can be used for neoadjuvant patients waiting to receive subsequent therapy or to identify patients that might be at higher risk for a specific study-determined endpoint while receiving a curative intent intervention.
#5 ctDNA monitoring supports earlier detection of existing and new alterations that indicate the emergence of resistance mechanisms
Dr. Cohen explained that these assays are quantitative at the molecular level, enabling the identification of existing and new alterations that are likely to portend resistance. “Liquid biopsy testing can inform the modification of patient treatment with EGFR inhibitors for non-small cell lung cancer, for example,” said Dr. Cohen.
ctDNA enables monitoring of tumor heterogeneity and detection of subclonal variations, providing a more comprehensive picture of the tumor composition and effectively guiding subsequent treatment decisions for patients at risk of developing resistance.
“We can begin to think about using ctDNA-based therapy response assessments for the discovery of novel agents and mechanisms of resistance, where these markers can be detected in real-time in ctDNA rather than having to collect tumor biopsies,” Dr Cohen said.
Furthermore, ctDNA-based monitoring enables time-sensitive treatment modification for late-stage cancer patients receiving immunotherapy. Liquid biopsy assaying evaluates the effectiveness of an intervention much faster and with higher sensitivity than traditional methods; changes in tumor size take anywhere from eight weeks to several months or longer to manifest on radiographs. Earlier readouts of ctDNA levels gained from liquid biopsies limit exposing patients to toxic treatments over time.
The future of liquid biopsy applications
As the utility of Tempus’ xF+ panel and — more broadly — liquid biopsy evolves, Dr. Beaubier and Dr. Cohen agreed there are many opportunities to expand genomic profiling capabilities across research and clinical development settings. Increasing the genomic space to investigate the tumor mutational and broader pathway landscape will streamline clinical program development, whether in early or late stages.
Dr. Cohen also hypothesizes that ctDNA and liquid biopsies will become the standard of care. “I think liquid biopsy and ctDNA will be standard practice in assessing a patient from the very first visit, as well as monitoring tumor burden or treatment response,” Dr. Cohen said. “For patients treated in the curative setting, liquid assays will give clinicians the opportunity to improve surveillance and detect recurrence sooner than conventional methodologies.”
Dr. Beaubier adds that broader datasets have the potential to uncover novel targets and additional actionable variants, she urges clinicians to remain vigilant for secondary insights. “In tumor normal-match, for example, we often see incidental germline findings related to things like cardiac risk which aren’t relevant for the primary investigation when running an oncology panel,” said Dr. Beaubier. “As such, it is crucial to remain alert and follow up on the data. Still, in my opinion, anything that detects disease earlier and provides clinicians and researchers something to take action on is fantastic.”
If you have questions about xF+ or how to apply liquid biopsy testing in your research or clinical programs, please contact the Tempus team here.
-
12/11/2025
Driving enterprise value with RWD
Hear from biotech CEOs and VC leaders as they discuss how real-world data can inform strategic decision-making in biotech companies.
Watch replay -
11/11/2025
A new era of biopharma R&D: The TechBio revolution—realities and the next frontier
Join Tempus and Recursion leaders to explore their strategic TechBio partnership. Learn how they use AI and supercomputing with petabytes of data to accelerate drug discovery and development. See the impact on biopharma R&D's future.
Watch replay -
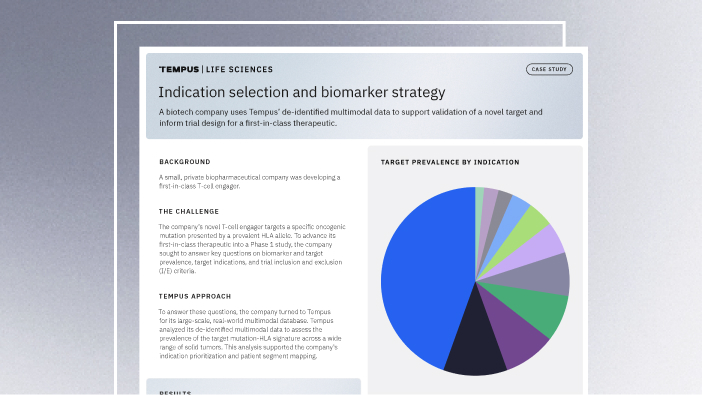
11/14/2025
Validating a novel target and informing trial design for a first-in-class therapeutic
Discover how a biopharma company used Tempus’ de-identified multimodal data to support validation of a novel target and inform trial design for a first-in-class therapeutic.
Read more